Closing the Information Gap in Medicine: How PByT Supports Better Clinical Decision-Making Through Real-Time Feedback
For clinicians, accurate information is the foundation of safe and effective medical practice. Yet today’s health-care environment is shaped by information bottlenecks, commercial pressure, and regulatory structures that lag far behind clinical reality.
The result is a system where doctors are expected to make high-stakes decisions without timely, reliable, real-world data.
The OxyContin crisis remains the clearest example of what happens when this gap is exploited. Purdue Pharma’s fabricated research, manipulation of regulatory pathways, and aggressive marketing created a false perception of safety that shaped prescribing behaviour across the profession. When the truth emerged, the damage was catastrophic: millions harmed, communities devastated, and trust in the health-care system profoundly shaken.
Even more troubling, the structural weaknesses that allowed this to occur remain largely unaddressed. No senior Purdue executives or Sackler family members faced jail time, and the systems meant to safeguard clinicians and patients have not fundamentally changed.
Similar patterns are visible today:
- The rise of vaccine hesitancy, now contributing to outbreaks of diseases once thought eradicated.
- The aggressive promotion of GLP-1 drugs as a fast solution to obesity, far outpacing long-term safety data.
- The widespread use of hair-loss drugs like Finasteride, where real-world side-effect profiles remain poorly understood, especially among young men.
At the core of each issue is the same structural failure:
The Structural Problem: A Data Vacuum in Day-to-Day Clinical Practice
Clinicians rely on regulatory approvals, published research, guidelines, and professional education. But these inputs are often slow, incomplete, or susceptible to commercial distortion.
Purdue exploited a fundamental weakness: the absence of real-time, real-world clinical data that practitioners can independently verify.
When evidence is falsified or incomplete, and when regulators fail to detect manipulation, clinicians are left without the tools to accurately assess risk–benefit profiles—particularly for newly introduced or heavily marketed treatments.
This is not a failure of the profession. It is a systemic vulnerability created by the way medical information is gathered, filtered, and distributed.
A Practical Solution: PByT’s Real-World Evidence Platform
PByT (Powered by Trust) introduces a global, analyzable feedback system designed to capture real-world outcomes from both patients and practitioners—closing the information gap that has repeatedly placed clinicians in harm’s way.
This tool provides clinicians with:
- Real-time visibility into patient-reported outcomes, treatment efficacy, and side-effect patterns
- Dynamic charts and analytics to rapidly identify emerging trends
- Transparent, global datasets not shaped by commercial marketing
- A structured way to contribute clinical insight, anonymously or publicly
PByT does not replace clinical trials. It complements them—providing ongoing, post-market surveillance generated by the people who actually prescribe and use medical products.
For clinicians working under time pressure, PByT becomes a fast, independent checkpoint to verify assumptions and strengthen confidence in treatment decisions.
Independent Research Through the Global Social Capital Fund
A long-standing dilemma in medicine is the heavy reliance on pharmaceutical-funded research. Even when conducted ethically, the incentives create unavoidable conflicts of interest.
The Global Social Capital Fund (GSCF), PByT’s economic pillar, offers an alternative by:
- Funding independent research to validate or challenge pharmaceutical claims
- Supporting neglected therapeutic areas overlooked by commercial interests
- Providing resources for legal action where fraudulent practice is uncovered
This strengthens the evidence base without increasing costs or burdens for clinicians.
Reducing Risk for Ethical Pharmaceutical Companies
For companies committed to scientific integrity, PByT offers a valuable advantage.
Transparent, real-world feedback:
- Reduces litigation risk
- Validates product performance
- Strengthens trust with prescribers and regulators
In a climate of increasing scrutiny, the ability to demonstrate independent, real-world outcomes is an asset—not a threat.
Early Clinical Focus Areas: Vaccines, Finasteride, and GLP-1 Therapies
The first three PByT hubs address areas where uncertainty, misinformation, or rapid uptake have created heightened risk:
Vaccines
Declining confidence driven by misinformation is leading to outbreaks of measles, whooping cough, and other preventable diseases. Transparent feedback helps correct false beliefs and highlight real patterns in safety and effectiveness.
Finasteride
Debate over the prevalence and severity of sexual, emotional, and neurological side effects—especially among young men—remains unresolved. Real-world feedback provides a clearer evidence base for prescribing decisions.
→ Have your say on Finasteride.
GLP-1 weight-loss drugs
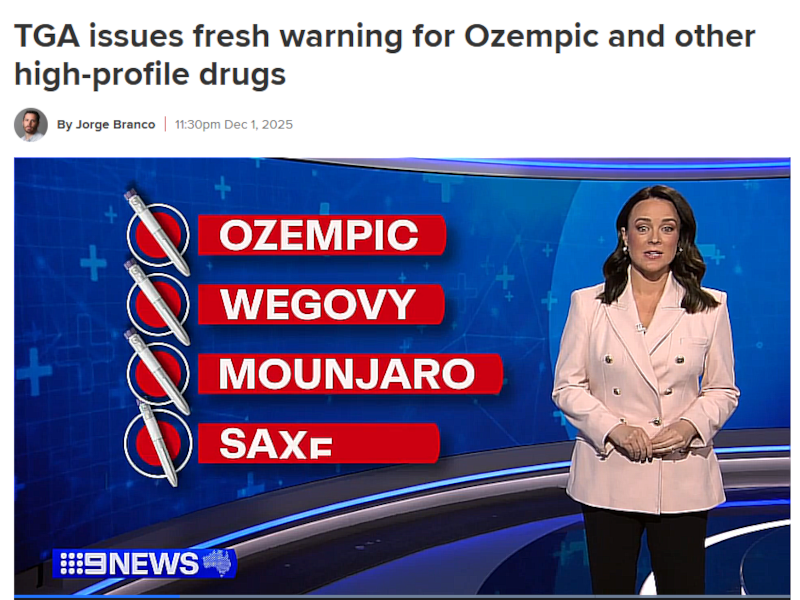
Ozempic, Wegovy, Mounjaro and similar drugs are being adopted faster than long-term research can keep up. Clinicians urgently need unbiased, real-world data on side effects, discontinuation rates, and long-term outcomes.
By gathering verified experiences, PByT helps clinicians understand what is happening at scale—not filtered through marketing campaigns or anonymous online anecdotes.
→ Have your say on GLP-1 drugs.
A Modern Tool for a Modern Profession
The systemic failures of the past—from OxyContin to off-label incentive schemes—were not caused by clinicians but by a system that restricted access to accurate, timely information.
PByT strengthens clinical practice by:
- Improving access to real-world evidence
- Providing independent verification mechanisms
- Reducing reliance on marketing-driven information
- Enhancing patient trust and communication
- Supporting stronger clinical governance
In short, PByT helps realign clinical judgment, patient outcomes, and transparent information.
This is not just another digital platform. It is a modern safety net for clinicians—a safeguard designed to prevent the next OxyContin-level catastrophe.


